Several studies have shown that keeping your baby close to you at night helps everyone get more rest and results in longer breastfeeding duration.
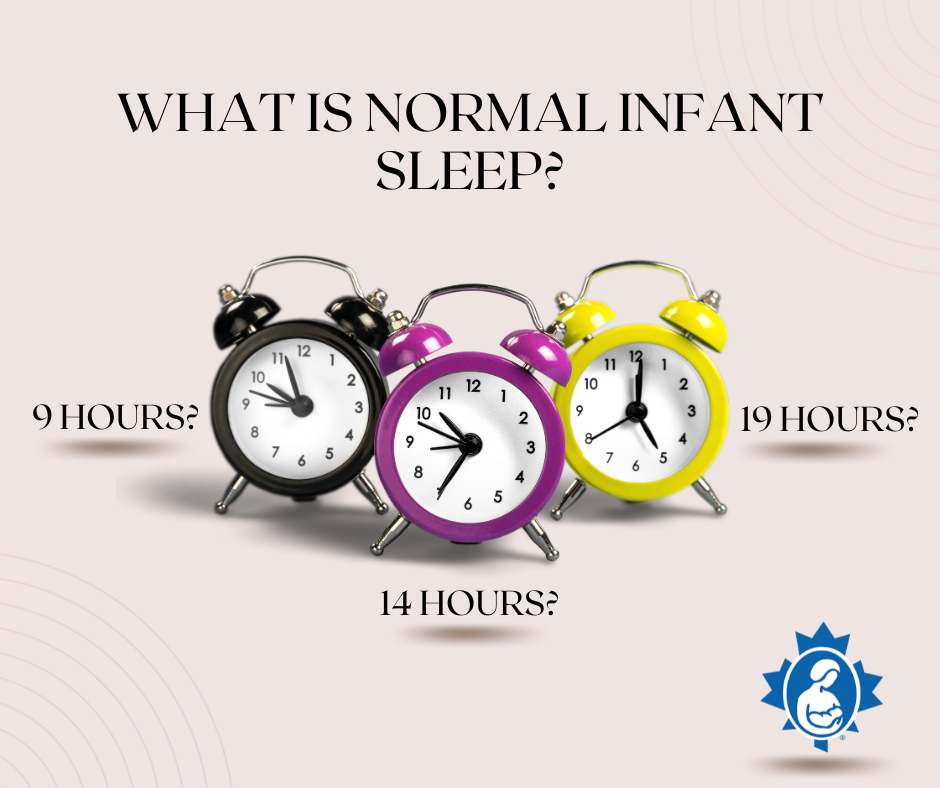
There is a wide range of what is a normal amount of sleep for a newborn baby. Normal can be anywhere from nine hours to nineteen hours of sleep per day. The average is fourteen hours per day. Babies do not even begin to develop their circadian rhythm (sleeping more at night than during the day) until around three months of age.
Studies show a wide variation in infant sleep in the first two years of life. Some babies may start to sleep longer stretches (about six hours at night) by around six months of age. However, at one year many babies continue to wake two, three or more times at night. They are usually nursing for nutrition, sometimes for comfort. After one year of age babies are more likely to gradually sleep longer stretches at night. But for some babies this may not happen until closer to two years or later. Each baby’s sleep pattern is individual.
Babies sleep a lot but they also wake frequently - for very good reasons. Frequent waking protects young babies from SIDS (Sudden Infant Death Syndrome) and makes sure they feed often. See SIDS Prevention and Breastfeeding.
Remember that frequent feedings are normal and important. Frequent waking means frequent feedings, day and night. This allows babies to get all the milk they need to grow and thrive. When your breasts are emptied regularly, your body gets the signal to make more milk. See Establishing Your Milk Supply for more information.
Newborns feed frequently - sometimes at regular intervals and often at irregular intervals. For most newborns, the longest stretch is between three or four hours. It can be helpful to remember night waking is normal and beneficial for babies.

Breastfeed at night following baby’s needs
A study done at the University of California showed that parents of infants who were breastfed in the evening and/or at night slept an average of 40-45 minutes more than parents of infants given formula. Parents using formula at night also self-reported more sleep disturbance than parents of infants who were exclusively breastfed at night.
Many parents are more relaxed about their baby’s sleep when they realize that each baby has her own sleep pattern. There is no set number of hours that babies need to sleep. Waking several times at night is common, especially in the early months.
If you are tired, rather than trying to change your baby’s sleep, consider trying to find ways for you to get more rest during the day and at night.
- Sleep when your baby sleeps, as much as possible.
- Ask a support person to care for your baby in your home first thing in the morning, right after your baby has nursed. Many mothers find this helpful because it is easier to drift back to sleep than to try to sleep once you’ve been awake for a while.
Keep your baby close
When your baby senses that you are nearby, your baby’s stress levels stay low. Low stress levels promote growth. Your baby sleeps comfortably knowing you are close. And you sleep comfortably knowing that your baby is next to you. When your baby begins to wake, you can move her to your breast quickly, before she cries. It is much easier to nurse a calm baby.
Studies have shown that babies who sleep near their mothers at night are more likely to breastfeed than those who sleep in different rooms. Babies who sleep in their mothers’ beds are the most likely to be breastfeeding at various ages. And mothers who follow strict feeding and sleep practices are least likely to breastfeed.

Your baby will want to be near you during the day. Wearing your baby safely in a ring sling, wrap or front carrier can allow your baby to feel close. And it gives you the freedom to do what you need to do - make yourself a sandwich, fold laundry or go for a walk while your baby is sleeping happily next to you. Baby wearing is also helpful if your baby prefers to drift off to sleep with some movement.
When wearing your baby, it’s important to use a carrier that allows your baby to be in a safe, upright position.
- You can kiss your baby’s head and see her face (visible and kissable.)
- Your baby has a straight back.
- Your baby can sleep with her head turned to one side, on your chest and her feet near your belly.

If you are feeling tired when your baby is in the carrier, sit down and adjust your baby as needed. Your baby should be upright in the carrier while you relax (see point above). If you are very sleepy, it is better to take your baby out of the carrier and lie down side by side on a safe sleep surface. (See Safe Sleep Surface Checklist, below.)
Another option is to put your baby in a stroller and go for a walk. Your baby may drift off to sleep with the movement of the stroller. And you can get some fresh air and exercise while your baby naps. Or you may want to go for a drive with your baby safely in the infant car seat. The movement of the car can help your baby fall asleep.

For those times when you want to put your baby down, but not sleep yourself, it’s helpful to have a safe sleeping surface in the main living area, where you spend most of the day. If you can see and hear your baby, you can get to your baby within seconds if she signals that she needs you.
Many mothers nurse their babies to sleep on a safe sleeping surface and then move away after their babies are asleep. Others will nurse their babies to sleep either sitting up or lying down and continue to stay with their baby to sleep, read, look at their phone or watch TV.
Consider safe bedsharing
Bedsharing is the term used when parent and baby sleep together on the same surface. (Co-sleeping is when parent and baby sleep near each other in the same room.) In many countries it is the usual way to care for babies and toddlers at night. Babies are soothed by being close to their parents. Everyone gets more sleep.
Not all breastfeeding families bedshare. However, mothers who don’t plan to bedshare often end up doing it accidentally when they fall asleep while breastfeeding. So even if you are not planning to bedshare, it’s important to make your bed a safe sleep surface.
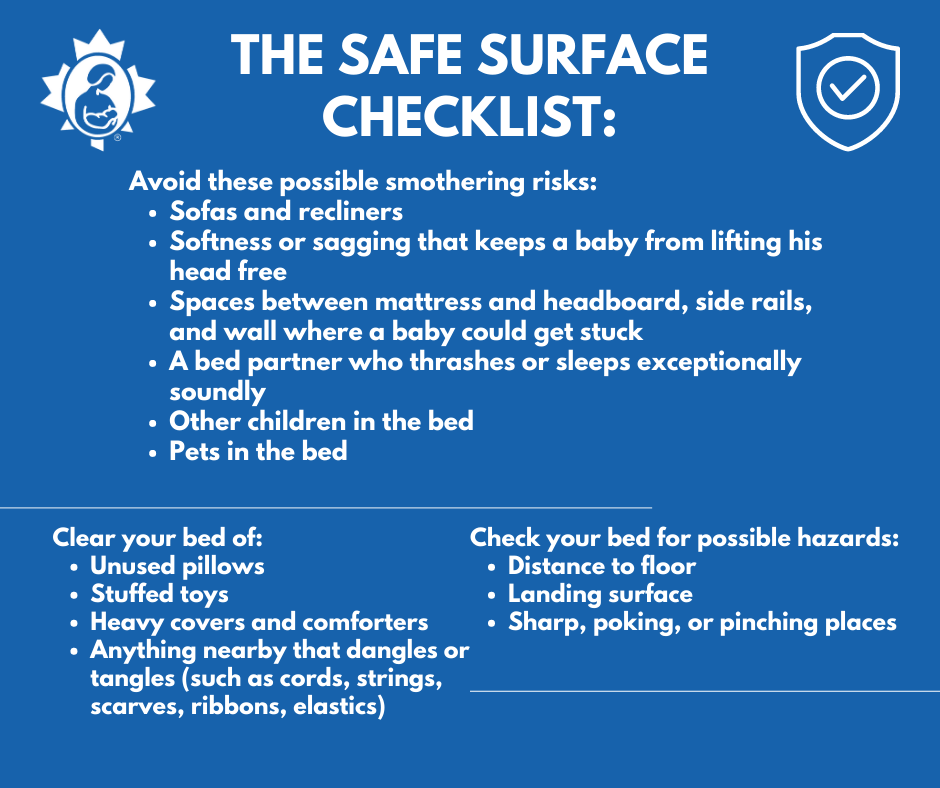
If you decide to bedshare with your baby, it's important to do it safely. See the Safe Sleep Seven and the Safe Surface Checklist below.
If you can meet the Safe Sleep Seven criteria and the Safe Surface Checklist, then solid research indicates that your baby’s SIDS risk is no greater in your bed than in a crib. And your automatic behaviors and responsiveness as a breastfeeding mother make it practically impossible for you to roll over on him. Dr. James McKenna uses the term breastsleeping to describe how breastfeeding mothers and babies sleep together.

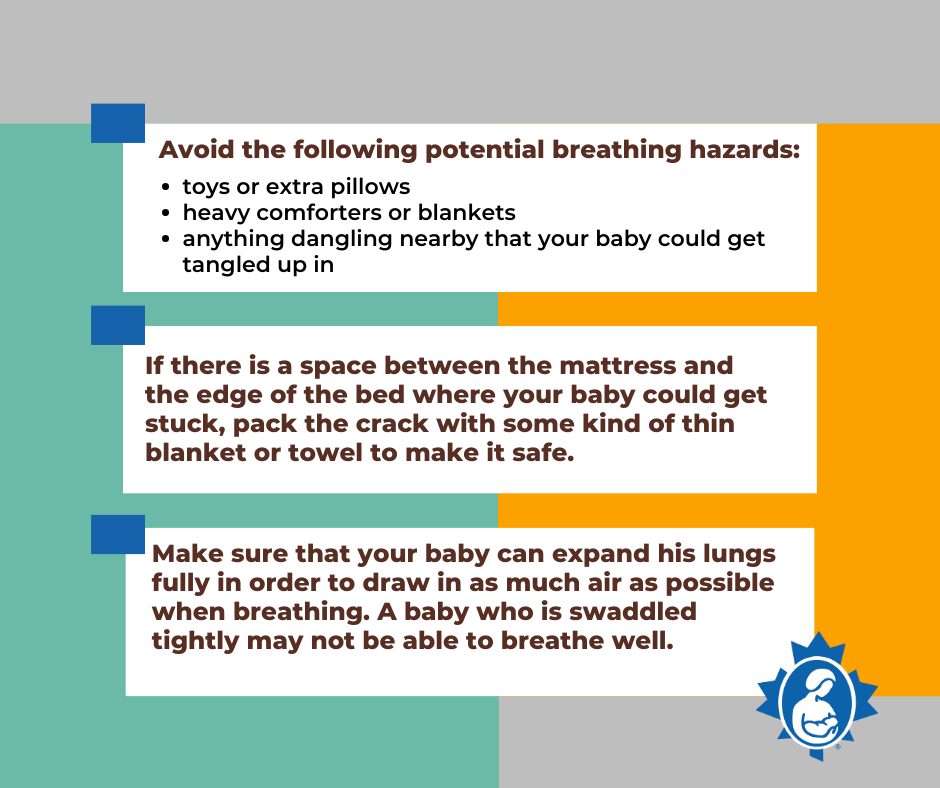
Whether your baby sleeps in your bed or on a separate sleep surface, you’ll want that sleeping space to be safe. Sadly, babies can die unexpectedly when they suffocate or are smothered while sleeping. Suffocation/smothering deaths are not the same as Sudden Infant Death Syndrome (SIDS) where the cause of death is unknown.
Babies are surprisingly good at moving around even when they are small. It is very important to avoid any breathing hazards when your baby is sleeping.
Keep things quiet and dark at night
Consider not changing your baby’s diaper at night, unless it is poopy. Use a barrier cream on your baby’s bottom before bed. A breathable waterproof mat under you and your baby can absorb milk and diaper leaks. Breastfed babies often do not need to be burped. If you do need to burp your baby, there is no need to sit up. While you are lying on your side, place your baby up over your waist. And do your best to leave the lights off. This will help both you and your baby to get back to sleep.

In the La Leche League International publication Sweet Sleep: Nighttime and Naptime Strategies for the Breastfeeding Family, the authors explain how and why many breastfeeding mothers can bedshare responsibly. The heart of this book is the “Safe Sleep Seven” – seven criteria that create that level of safety. These clear criteria offer reassurance to many parents and give them a way to evaluate the risk in their own situation. Preparing your bed for bedsharing – whether you plan to bedshare or not – is your first childproofing job because sleep happens, starting on Night One.

The Safe Sleep Seven and The Safe Surface Checklist are from Sweet Sleep: Nighttime and Naptime Strategies for the Breastfeeding Family Copyright © 2014 by La Leche League International, Diane Wiessinger, Diana West, Linda J. Smith, Teresa Pitman. 512 pages.
Resources for Parents
Basis: Baby Sleep Info Source, UK.
Mother Baby Behavioral Sleep Laboratory
References
Bartick, M., Young, M., Louis-Jacques A., McKenna, J.J. and Ball, H.L. (2022). Bedsharing may partially explain the reduced risk of sleep-related death in breastfed infants. Frontiers in Pediatrics, 10:1081028. doi:10:3389/fped.2022.1081028
Basis: Baby Sleep Info Source, UK
Blair, PS et al. Bedsharing and Breastfeeding: The Academy of Breastfeeding Medicine Protocol #6, Revision 2019
Blair, P.S., Heron, J., Fleming, P.J. (2010). Relationship between bed sharing and breastfeeding: longitudinal, population-based analysis. Pediatrics. Nov;126(5):e1119-26. doi: 10.1542/peds.2010-1277
Bovbjerg ML, Hill JA, Uphoff AE, Rosenberg KD. (2018). Women Who Bedshare More Frequently at 14 Weeks Postpartum Subsequently Report Longer Durations of Breastfeeding. J Midwifery Womens Health, Jul;63(4):418-424. doi: 10.1111/jmwh.12753
Doan, T., Gardiner, A., Gay, C.L., Lee, K.A. (2007). Breast-feeding Increases Sleep Duration of New Parents. Journal Perinatal and Neonatal Nursing, Jul-Sep;21(3):200-6. doi: 10.1097/01.JPN.0000285809.36398.1b
Harries, V, Brown, A. (2019). The association between baby care books that promote strict care routines and infant feeding, night-time care, and maternal–infant interactions. Maternal and Child Nutrition, 15(4). https://doi.org/10.1111/mcn.12858.
Howel D, Ball H. (2013). Association between length of exclusive breastfeeding and subsequent breastfeeding continuation. Journal of Human Lactation. Nov; 29(4): 579-85. doi: 10.1177/0890334413492908
Okami, P., Weisner, T., Olmstead, R. Outcome correlates of parent-child bedsharing: an eighteen-year longitudinal study. (2002). Journal Developmental and Behavioral Pediatrics, Aug; 23(4):244-53. doi: 10.1097/00004703-200208000-00009
Pitman, T., West, D., Wiessinger, D. (2014). Sweet Sleep: Nighttime and Naptime Strategies for the Breastfeeding Family.
Pennestri, M-H., Laganière, C., Bouvette-Turcot, A-A., Pokhvisneva, I., Steiner, M., Meaney, M.J., Gaudreau, H. (2018). Uninterrupted Infant Sleep, Development, and Maternal Mood. Pediatrics, 142(6): e20174330. https://doi.org/10.1542/peds.2017-4330
Srimoragot, M., Hershberger, P. E., Park, C., Hernandez, T. L., & Izci Balserak, B. (2023). Infant feeding type and maternal sleep during the postpartum period: a systematic review and meta-analysis. Journal of Sleep Research, 32(2), e13625. https://doi.org/10.1111/jsr.13625
Vennemann, M.M., Bajanowski, T., Brinkmann, B., Jorch, G., Yücesan, K., Sauerland, C., Mitchell, E.A. (2009). Does breastfeeding reduce the risk of sudden infant death syndrome? Pediatrics; 123(3):e406-10. Doi: 10.1542/peds.2008-2145.
Updated 2024
