
Breastfeeding protects babies from SIDS
Sudden Infant Death Syndrome (SIDS) or “crib death” is the unexpected and unexplained death of a baby. SIDS can occur any time in the first year. The time of highest risk is between one to six months. Suffocation/smothering occurs when a baby cannot breathe. This is not the same as SIDS. SIDS deaths are unexplained.
Biggest risk factors for SIDS
- smoking
- laying a baby facedown for sleep (prone)
- leaving a baby unattended
- formula-feeding (Sweet Sleep, p.345)
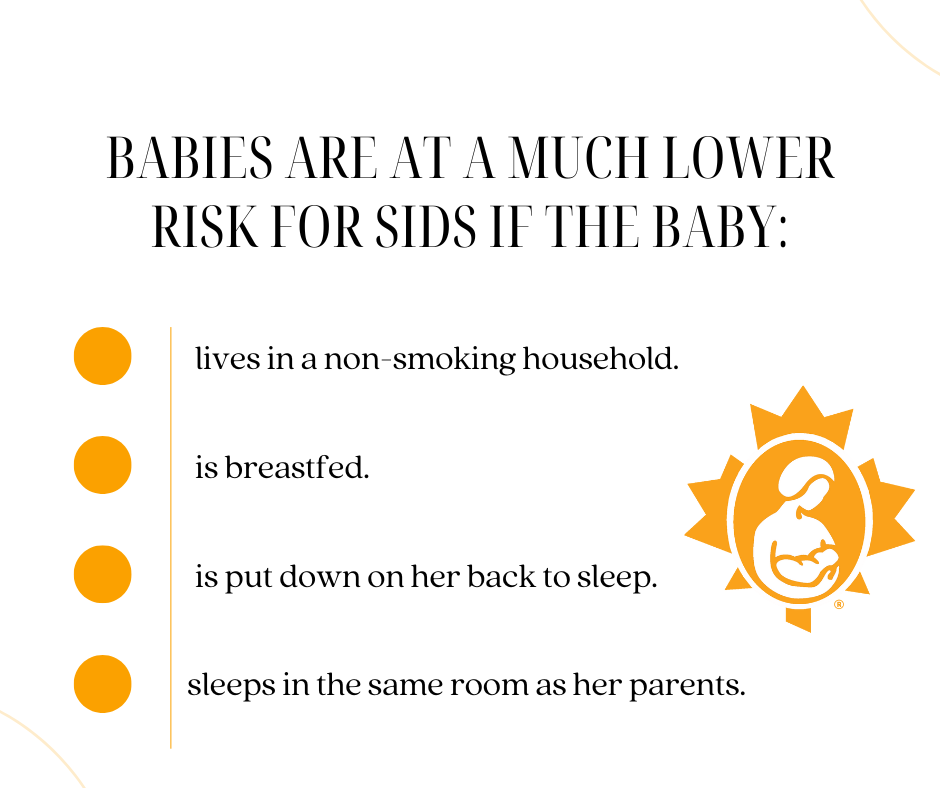
Regardless of how you feed your baby or where you and baby sleep, putting your baby to sleep unswaddled on his back is the safest option.
Smoking cigarettes
It’s important to know that if you are going to smoke cigarettes or use e-cigarettes (‘vape’), the best thing you can do for your baby is breastfeed. Nursing helps to minimize some of the negative effects that smoking can have on your baby. If you use nicotine, even if you never smoke around your baby or always smoke outdoors, it is recommended that you not share a bed with your baby. Instead, put your baby to sleep in a bassinet or crib in the same room, but not right next to your bed. With your baby in the same room as you, you can easily get to your baby during the night for feedings. See Smoking, ‘Vaping’, Nicotine and Breastfeeding for more information.
Waking frequently protects against SIDS
Frequent waking during the night helps babies to rouse themselves if they have sleep apneas (stopping breathing).
Researchers suspect that babies who die of SIDS do so because they have trouble rousing out of deep sleep. Sadly, many of the techniques that parents use to try to get their babies to sleep longer actually increase the risk of SIDS. Thus, it’s important to avoid:
- giving your baby a big bottle of formula before bed.
- putting your baby in a warm room alone away from any arousing noises you might make in the night.
- tightly swaddling your baby.
- putting your baby on their tummy to sleep.
Getting enough sleep while supporting your baby’s need to wake frequently at night helps to:
- protect your milk supply.
- prevent SIDS.
- keep your baby calm and relaxed through the night.
See Sleep and the Breastfeeding Family.
Sleeping near your baby protects against SIDS
Breastfeeding mothers who sleep with their babies within arm’s reach are deeply in tune with their babies even when both are asleep. Your movements, breathing and noises, while adjusting your position, keeps your baby from falling into a deep sleep state. Some babies have difficulty waking from a deep sleep.
Breastfeeding mothers who bedshare, or sleep in the same bed as their babies, usually sleep facing their babies. They have one arm above their baby’s head and their body curled around their baby. (Dr. James McKenna calls this “breastsleeping.”) After feeding, mothers can roll their babies away from the breast onto their backs. This is the safest sleep position for SIDS prevention.
Bedsharing
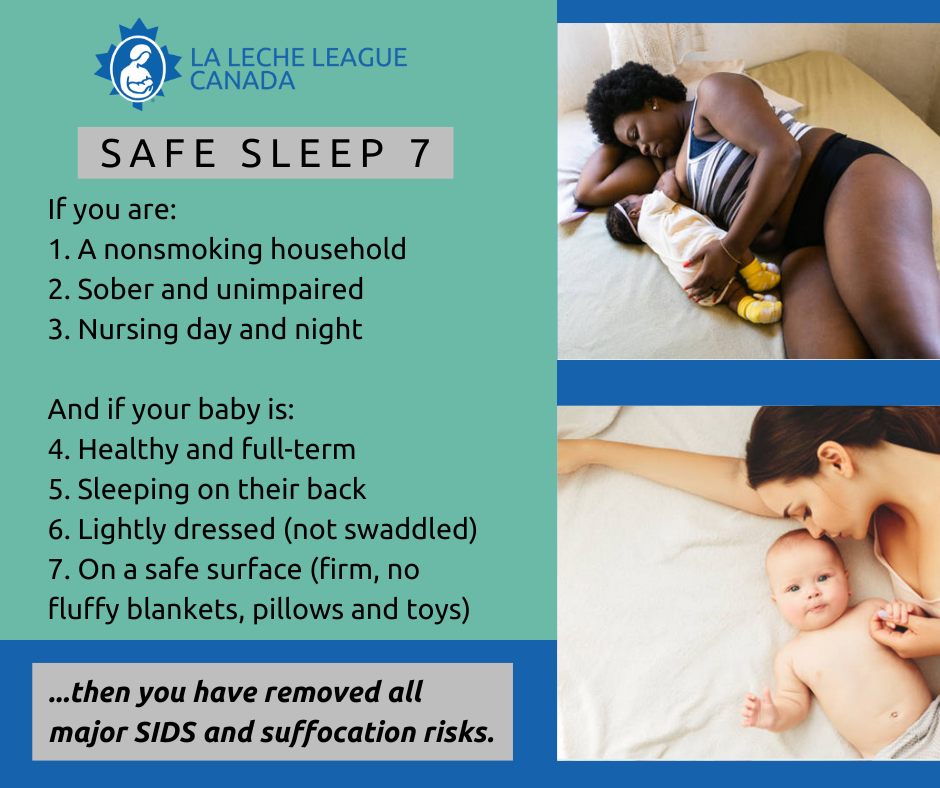
Health Canada recommends not bedsharing with your baby. However, many breastfeeding mothers bring their babies in bed with them for all or part of the night. Health Canada recognizes this and provides information about how to bedshare safely. The National Health Service in the UK recommends bedsharing as long as it is done safely. Parents who bedshare safely follow the Safe Sleep Seven.
Many studies have shown that bedsharing increases breastfeeding rates and increases nighttime waking. Both breastfeeding and frequent night-waking are protective against SIDS. Studies also show that mothers who bedshare get more sleep, even though their babies wake more frequently.
The Safe Surface Checklist:
- Avoid these possible smothering risks:
- Sofas and recliners.
- Softness or sagging that keeps a baby from lifting his head freely.
- Spaces between a mattress and headboard, side rails, and a wall where a baby could get stuck.
- A bed partner who thrashes or sleeps exceptionally soundly.
- Other children in the bed.
- Pets in the bed.
Clear your bed of:
- unused pillows.
- stuffed toys.
- heavy covers and comforters.
- anything nearby that dangles or tangles (such as cords, strings, scarves, ribbons, elastics)
Check your bed for possible hazards:
- Distance to floor.
- Landing surface.
- Sharp, poking, or pinching places.
The Safe Sleep Seven and The Safe Surface Checklist are from Sweet Sleep: Nighttime and Naptime Strategies for the Breastfeeding Family.
Resources for Parents
Basis: Baby Sleep Info Source, UK.
LLLI: Bedsharing and Breastfeeding
Mother Baby Behavioral Sleep Laboratory
References
Bartick, M., Young, M., Louis-Jacques A., McKenna, J.J. and Ball, H.L. (2022). Bedsharing may partially explain the reduced risk of sleep-related death in breastfed infants. Frontiers in Pediatrics. 10:1081028. doi:10:3389/fped.2022.1081028
Blair, P.S., et al. Bedsharing and Breastfeeding: The Academy of Breastfeeding Medicine Protocol #6, Revision 2019.
Health Canada. (February 10, 2023). Safe Sleep for Your Baby.
National Health Service, United Kingdom (NHS). Reduce the risk of sudden infant death syndrome (SIDS). (November 15, 2021).
Pitman, T., West, D., Wiessinger, D. (2014). Sweet Sleep: Nighttime and Naptime Strategies for the Breastfeeding Family.
Vennemann MM, Bajanowski T, Brinkmann B, Jorch G, Yücesan K, Sauerland C, Mitchell EA; GeSID Study Group. (2009, March). Does breastfeeding reduce the risk of sudden infant death syndrome? Pediatrics;123(3):e406-10. Doi: 10.1542/peds.2008-2145. PMID: 19254976.
Updated 2024
