
(The following article is a summary of information found in the Academy of Breastfeeding Medicine Clinical Protocol #36: The Mastitis Spectrum, Revised 2022)
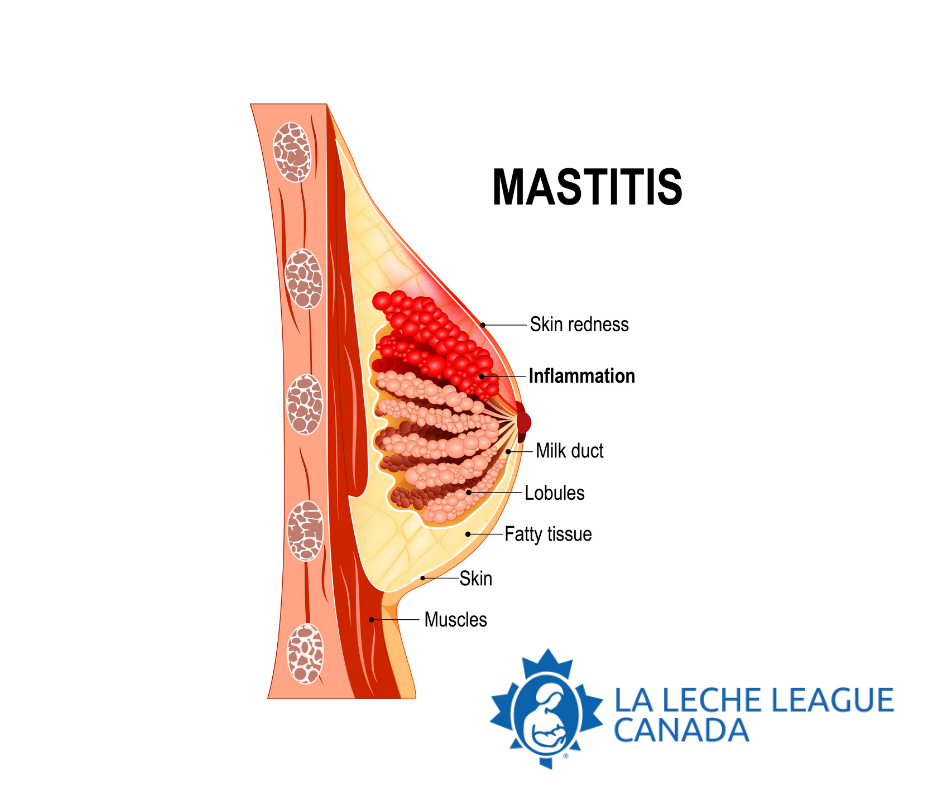
Mastitis is the name given to a range of conditions that all involve inflammation in the breast. You may never experience mastitis or you may find that you need to take steps to prevent it from recurring.
As you produce milk, some of the many, many small ducts (tubes) that transport your milk can get overly full. You may occasionally feel discomfort or tenderness that gets better after your baby nurses or you express some milk. If you notice an area that is hard, swollen, warm, painful or red (on lighter skin tones) that isn’t relieved by nursing or pumping, one or more of those ducts may have become inflamed.
The good news is that with supportive care mastitis does get better and you can continue to breastfeed through it all. Mastitis usually starts with a simple inflammation in just one milk duct which causes the duct to narrow, slowing down the flow of milk. This has often been called a “plugged” duct; since there isn’t really a “plug,” this term can be misleading. Mastitis may also involve a much larger area of inflammation in the breast tissue. You may feel achy, with fever, chills and a rapid heartbeat, similar to having the flu. Sometimes this inflammation goes on to become a bacterial infection, which may require antibiotic treatment. Mastitis is not contagious. You don’t need to routinely sterilize pump parts, pacifiers or household items. Early treatment to reduce the inflammation can help you avoid an infection. All stages of mastitis are treatable.
If your breasts are engorged, reverse pressure softening along with hand expression of small amounts of milk will make it easier for your baby to latch.
If your breast is really sore, or you’re feeling achy and rundown, it can be hard to stay motivated about nursing your baby. Get as much rest as possible, do what you can to reduce any stress in your life, and reach out to a La Leche League Canada Leader for support.
What to do?
● Nursing or expressing milk regularly, following your baby’s cues, will help prevent the breast getting overly full. This is much easier if you keep your baby close to you. There’s no need to ‘empty’ your breasts beyond what your baby wants to drink.
● Positioning your baby with their chin in line with the sore area can help them remove milk more effectively from that spot.
● The following are ways others have found helpful to decrease inflammation and pain:
○ Apply ice/cold packs every hour or more often, if it feels good.
○ Consider using a nonsteroidal anti-inflammatory drug like ibuprofen to relieve inflammation and pain.
○ Consider using a pain-relieving drug like acetaminophen, as needed.
○ Consider taking lecithin supplements (soy or sunflower) which can reduce the stickiness of milk fat. For how much to take, follow the instructions on the package. The Academy of Breastfeeding Medicine recommends 5-10 g/day. If you have questions about dosage, consult your healthcare provider.

● If your breasts are uncomfortably full, hand expressing small volumes of milk between feedings can provide some relief.
● Deep massage of your breasts can increase the inflammation and tissue swelling. Instead use light sweeping of your skin and a very gentle touch. See Lymphatic Massage Technique video.
○ Make 10 small circles at the base of your neck, just above your collarbone.
○ Make 10 small circles where your breast meets your underarm.
○ Sweep from your nipple toward your chest, collarbone and underarm.
● Wearing a well-fitted, supportive bra can be more comfortable.
● Taking probiotics, which can help reestablish the microbial balance in your body, may be helpful. If probiotics are used, they should contain specific strains shown to be effective against mastitis pathogens (see What’s Happening in the Breast below).
● To treat a nipple bleb (white bump on your nipple):
○ Talk to your healthcare provider about applying a topical steroid cream to the nipple. Lecithin supplements can help here too.
○ Avoid salt water soaks, castor oil rubs, and other topical products on your nipples.
○ Do not try to open the bleb. Most cases of mastitis resolve in a few days of using the strategies above. Contact a La Leche League Leader for additional support.

What if things aren’t improving?
If you are not starting to feel better after 24 hours and continue to have a fever and/or fast heart rate (tachycardia), talk with your healthcare provider about the possible use of antibiotics. Antibiotics are not recommended unless a bacterial infection is suspected. You can continue to nurse your baby while you are taking antibiotics.
Therapeutic ultrasound (TUS) uses thermal energy to reduce inflammation and may be an effective treatment for mastitis. This can be particularly useful for cases that do not resolve within a few days of trying other strategies. Trained physiotherapists can provide this service.
Sometimes mastitis progresses to a more serious condition called an abscess. This is where fluid collects in a well-defined area of the breast and becomes infected. In this case, surgical drainage becomes necessary. After aspiration or drain placement, you can continue breastfeeding from the affected breast. If hospital admission is necessary, talk to your healthcare provider about keeping your baby with you, so you can continue to breastfeed as often as your baby likes.
If you have recurring bouts of mastitis, ask your healthcare provider about culturing your milk to verify that there is a bacterial infection and/or to identify the pathogens responsible for the infection. It is also helpful to avoid long periods without feeding or expressing milk.
Remember that mastitis is treatable at all stages. Contact a La Leche League Leader or your healthcare provider if you suspect inflammation in your breast.
What’s happening in the breast?
Just like your baby’s gut, your breasts have a microbiome that works best with the right balance of microorganisms. Antibiotics and hyperlactation (too much milk) can disrupt that balance, resulting in inflammation and disruption of the milk microbiome (called mammary dysbiosis).
Use of Antibiotics and Probiotics
Treating inflammatory mastitis with antibiotics can change the normal bacterial balance in the breast and actually increase the risk of developing bacterial mastitis.
Of course, antibiotics may be needed to treat bacterial mastitis or may be prescribed for other reasons. When that’s the case, it may be helpful to take probiotics as well. If probiotics are used, they should contain specific strains shown to be effective against mastitis pathogens (‘germs’) (Limosilactobacillus fermentum, formerly classified as Lactobacillus fermentum, or, preferably, Ligilactobacillus salivarius formerly classified as Lactobacillus salivarius).
Too Much Milk (Hyperlactation)
If you produce more milk than your baby needs, you are more likely to experience the inflammation that can lead to disruption of the milk microbiome (mammary dysbiosis). Hyperlactation can be caused by frequently pumping more milk than a baby is taking (to build up a freezer stash, for example), or by regularly pumping until the breasts are “empty”. Mammary dysbiosis itself can lead to narrowing of the milk ducts and inflammation, which can lead to further disruption of the milk microbiome. If you are separated from your baby or are exclusively pumping, aim to produce only the amount of milk your baby needs and not more.
It’s important that pump flanges fit well, so pumping is comfortable and milk flows easily. Flanges that are the wrong size, suction that is too high, and pumping for too long can all cause damage to the nipple and breast tissue.
When exclusively pumping, the exchange of beneficial microorganisms between baby and breast doesn’t happen. This may increase your chances of developing mastitis.
Milk production can be downregulated (reduced) by avoiding pump use, and hand expressing small volumes of milk between feedings when your breasts feel uncomfortably full. If you are exclusively pumping, aim to pump only as much milk as your baby needs to grow well. For more information, please see LLLC's Information Sheet: How to Know Your Baby is Getting Enough Milk. Please watch this video to learn more about Hand Expression.
Nipple Shields
● Using nipple shields may increase inflammation. It’s best to avoid them. They do not address the underlying causes of breastfeeding problems. If you are having trouble latching your baby comfortably and effectively, contact a La Leche League Leader or International Board Certified Lactation Consultant (IBCLC) lactation consultant for support.
Remember that breastfeeding can and should carry on throughout treatment for mastitis. If you need information and support, La Leche League Canada is here to help. Find your local LLLC Group.
Please consider supporting LLLC.
For more information about mastitis and treatment options to share with your healthcare provider, see: Academy of Breastfeeding Medicine Clinical Protocol #36: The Mastitis Spectrum, Revised 2022
Prepared by La Leche League Canada, June 2022.
